*Individual results may vary
Things We Cannot Control
There are a couple of things that neither the surgeon nor the patient can control in any way. By making smart decisions based upon science, experience and common sense, we can minimize the risk of problems, but two things in particular are beyond our control. It is important to understand this prior to making any decisions regarding surgery.
Bottoming Out
Tissue Stretch
When an implant is placed into the breast, the breast tissue will stretch. Sometimes, the lower pole (portion) of the breast will stretch more than desired. This will result in a longer than desired nipple to fold (lower breast crease) distance, with most of the breast volume in the lower pole of the breast.* The nipple will be upturned, with less upper breast fullness. This overstretching of the breast is due to the biology of the patient’s own tissues and as such cannot be controlled. However, one can minimize the risk of this happening by not placing an implant into the breast that is larger than recommended based upon taking measurements of the soft tissue. This is called soft tissue-based planning. Sometimes this overstretching is minimal and not recognized by the patient, however, in some cases it can be significant and requires operative correction. Due to the fact that I rely heavily on the principles of soft tissue based planning to select implant size, the need for operative revision of this problem in my busy breast augmentation practice is very infrequent, averaging only once or twice per year.
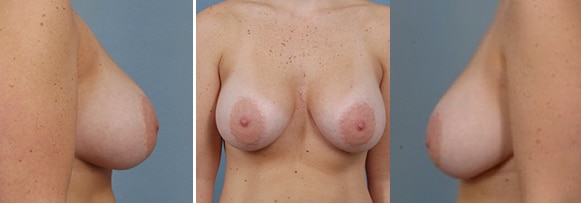
Mild Bottoming Out
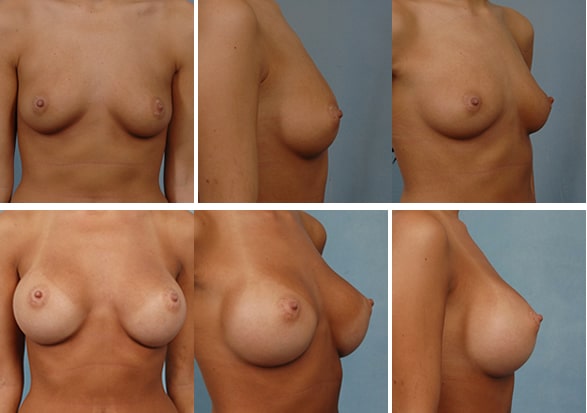
339 cc round silicone implants placed under the muscle. (Recommended size based upon measurements was 304 cc)*
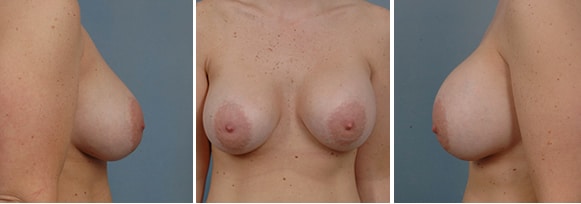
Moderate Bottoming Out
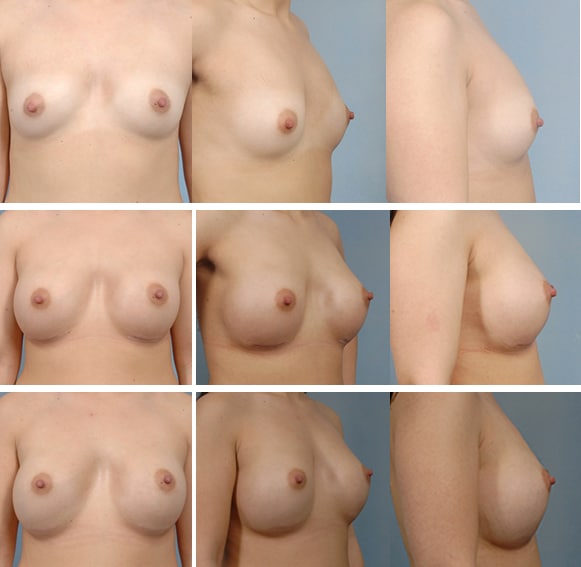
304 cc round silicone implants placed under the muscle. Post operative photos shown at 5 and 12 months after surgery.*
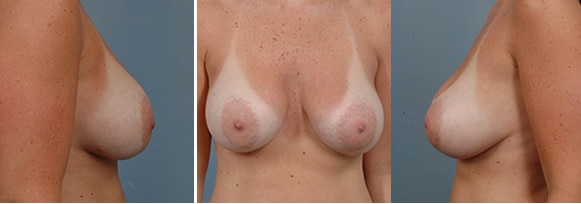
Severe Bottoming Out
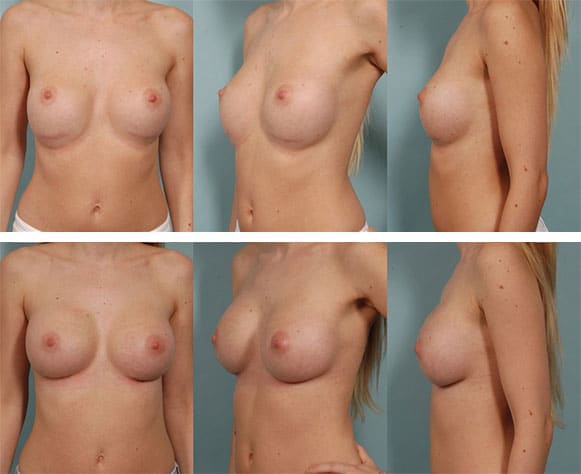
265 cc implants placed under the muscle. Despite the fact that this was the correct size implant for this patient, lower pole stretch can still occur, although rarely this severe. This was surgically corrected with a very good result.*
To view examples of surgical correction for “bottoming out,” click here.
Wound Healing/Scarring
Like almost every surgical procedure, incisions are a part of the breast augmentation and mastopexy process. In human skin, wherever you have an incision, a scar will form. Fortunately, breast augmentation and mastopexy scars, regardless of where they are located, tend to heal extremely well in the majority of patients. Scars can be hidden within a bra, bathing suit or low-cut top. During surgery, incisions are made in inconspicuous places on the breast to minimize scar visibility (in the armpit, in the crease on the underside of the breast, or around the areola, the dark skin around the nipple). A mastopexy does add additional scars such as around the areola, and usually a vertical scar from the bottom of the areola down towards the lower breast crease. In some occasions, an incision is made in this crease as well.
It is important to remember that scar quality is heavily influenced by your individual tissue biology of wound healing and that this factor is out of your control as well as mine. Some patients just naturally make great scars, and some make less than ideal scars. In my extensive experience with breast augmentation, I have found that in the vast majority of patients, the scars are thin, fade nicely and are not an issue for patient and partner.I close all breast augmentation wounds with the same technique, designed to give the best possible scar. However, everyone has different biologic propensities for wound healing which cannot be altered. Most scars on the breast heal beautifully. All scars are permanent and visible, but the vast majority, once they heal in the crease, are faint enough that upon casual view of the breast they are not an issue. Everyone is given scar care instructions including the use of topical agents and scar massage.
Occasionally, the scars are thickened and more visible (hypertrophic scar). Fortunately, this occurs rarely. Often times, this can be improved, although not eliminated, with steroid injections into the scar itself. I also employ the use of lasers and intense pulse light treatments to reduce the redness and soften the scars. This takes only a few moments and monthly treatments can be started as early as 4 weeks after surgery. Usually 4 – 6 sessions are required. There is a lot that that I do to minimize the visibility of the scars, but I cannot eliminate them completely. Scars do fade with time. The ultimate result is a combination of the plastic surgical techniques that I use to close the wound, your natural biology of wound healing, a factor that neither you nor I can control as well as the aftercare that you and I give the scar.
Capsule Contracture
On the inside of the breast there is scarring as well. The body responds to the placement of any foreign body, breast implant or otherwise, by forming scar tissue around the implant. This is called a capsule. In the vast majority of cases the capsule is thin and pliable, and is neither visible nor palpable and does not affect the aesthetic result of the augmentation in any way*. However, if stimulated, possibly by infection or blood around the implant, this scar capsule can become thickened and contract. As it contracts, the breast implant is deformed into a rounder shape, and the breast appears rounder, higher, and becomes firmer to touch. Occasionally, in very rare instances, the breast may be very tender as well. The problem is not the breast. It is not the implant. It is the scar tissue contracting tightly around the implant. Treatment consists of removing the implant and the scar tissue, either in whole or in part, and then replacing the implant. In very rare cases, if a woman has this problem happen twice to the same breast, I would recommend removal of the breast implants and not replacing them. So far, I have never been in a position to make this recommendation. It is believed by some that the further risk for scar capsule contracture may be increased after the first episode. I have not personally seen this in my practice, but I feel that it is worth mention. However, if the capsule contracture is mild, nothing other than observation need be done.
One of the main theories for why capsular contracture occurs is that blood accumulation around the implant after surgery acts as a culture medium for low virulent (potency) bacteria that settle in a film of tissue around the implant, safe from the body’s defenses, and stimulates this process. Using a minimally traumatic technique of surgical dissection which results in negligible blood loss during and after surgery, accompanied by several proactive means to prevent infection, including using three separate antibiotics plus Betadine (an antiseptic) in the solution used to wash out the breast pocket and soak the implant prior to use, capsule contracture has been an extremely rare complication in my practice. One interesting fact to note – use of the peri-areolar (nipple) incision for breast augmentation has been associated with an increased risk of capsule contracture, presumably due to the microorganisms that live within the nipple ducts and may contaminate the surgical field and breast implant during the surgery.