MYTH DISPELLED: IMPLANTS DO NOT LIFT THE BREAST!
This is important to get out of the way in the beginning. Many women are under the impression that getting a lift will solve the problem of a sagging breast. Many years ago, my wife was told this and ended up with implants that she did not want nor need. Small breast volume and sagging breasts are two different problems. They can be dealth with at the same time, but it is important to understand what changes an implant will make to the breast, and also what changes a lift will make to the breast. This is fundamental to breast surgery.
The Problem: Breast Drooping
True Ptosis versus False Ptosis (Pseudoptosis)
In my breast augmentation practice, a large portion of my patients are mothers who wish to restore lost volume to their breasts, or attain a volume that they wished they had previously. Many of these women have ptosis, or drooping, of their breasts. I already discussed the two types of ptosis: true ptosis and false ptosis, also known as glandular or pseudoptosis. True ptosis relates to the position of the nipple with respect to the lower breast crease, also known as the inframammary fold. False ptosis describes the position of the glandular tissue with respect to the inframammary fold. The degree of ptosis and pseudoptosis can vary independently with respect to one another as they are two separate entities. Unfortunately, they happen to have similar names which causes the confusion. Except for those women with very little breast tissue to start with, most all of these women have a combination of both types of ptosis.
The best surgical outcome will follow the most accurate assessment of the breast anatomy:
- Is there true ptosis, and if so, how severe
- Is there glandular ptosis, and if so, how severe
- What is the quality of the skin? The more overstretched and lack of elasticity, the harder it will be for the skin envelope to maintain good results. If one is also adding extra weight with an implant, this becomes even more significant. More on that later!
- How much breast parenchyma (glandular and fatty tissue) is there?
- What is the quality of the breast parenchyma (how firm is the tissue)?
- How much excess breast parenchyma is there in the lower breast. This is the tissue that sags. The more excess tissue in the lower breast, the harder it will be to obtain a lasting result. Sometimes this is dealt with by removing some of the excess tissue.
- Measurements of the breast (Clavicle to nipple, Sternal notch (top of the breast bone) to nipple, nipple to nipple, areolar diameter, nipple to lower breast crease) must be recorded.
As you can see there are several factors that need to be considered when deciding if a breast lift is indicated, and if so, which technique is best. There are no hard and fast rules. It is a judgment call based upon clinical experience. As a surgeon who has been performing aesthetic breast surgery for over thirty years, I have had a great deal of experience in seeing what works, what does not work and how to make the very best decisions for my patients. Below is a simplified version of how to think about when a breast lift is indicated. This applies whether or not breast implants are also being placed, although the specific technique chosen may vary depending upon whether or not breast implants are being placed at the time of breast lift.
Five Factors that Determine the Need for a Breast Lift:
- The amount of excess breast skin - the more excess skin, the greater the likelihood to need a lift
- The elasticity of the breast skin - the poorer the elasticity, the greater the likelihood to need a lift
- The amount of the breast tissue - the more breast tissue, the greater the likelihood to need a lift
- The firmness of the breast tissue - the softer the breast tissue, the greater the likelihood to need a lift
- The position of the nipple relative to the lower breast crease - the lower the nipple, the greater the likelihood to need a lift
If you envision a breast with an implant behind it, the breast tissue is pushed forward of that implant. Gravity is going to act on that breast tissue. The more factors that are unfavorable, the more the breast will sag and will thus need a lift to restore proper aesthetics to that breast.
With regard to the skin envelope, think of it as a ziploc bag. If the bag has a capacity for a gallon, but you fill it with only one quart of water, all the water will fall to the bottom of the bag, leaving the majority of it unfilled and sagging. Same thing with a breast. If the skin brassiere (the skin envelope) has a DD-cup capacity because that is the size you were while breast feeding, but now you only have a B-cup of breast tissue to fill it, the breast will appear empty and sagging. It is a common misconception to think that adding an implant to make up the difference will remedy the matter. Furthermore, an implant DOES NOT lift the breast. The problem is that the skin is overstretched and has poor elasticity. If you add a very large implant to fill out the breast, the nipple will appear too low, and the weight of this very large implant will now cause additional thinning out of the skin and stretching, and in a few months the breasts will look even worse! The answer here is to remove some of the breast skin (as is done with a breast lift) and make the skin envelope smaller with the nipple now in the proper position, use a smaller implant and get a much longer lasting result, maybe a C or D-cup with the breast properly filled out and the nipple positioned properly.
With regard to the breast tissue itself, the more breast tissue there is to start, the more it will be pushed forward of the implant. Gravity will act on this tissue, causing it to sag. The firmer the tissue, the more it will resist deformation of shape under the influence of gravity. The more tissue to start with, the firmer it must be to stay upwards.
The nipple position is also a very important factor. Ptosis, or drooping, is always assessed by looking at the nipple position in relation to the lower breast crease, also known as the inframammary fold. I do not care what the measurement is from the collar bone or the upper breast bone at the base of the neck to the nipple when assessing ptosis. Only the crease. Of course, I record these measurements, but more for symmetry purposes than any other reason. Very simply stated, the breast is like a hemisphere, and we want the nipple to be placed on the part of the breast that projects forward the most. This should be approximately the center of the breast. You cannot reference what the center is unless you can also see what the bottom of the breast is (where the lower breast crease is).
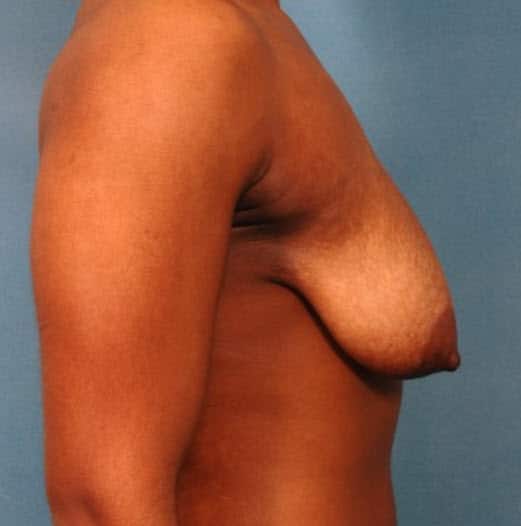
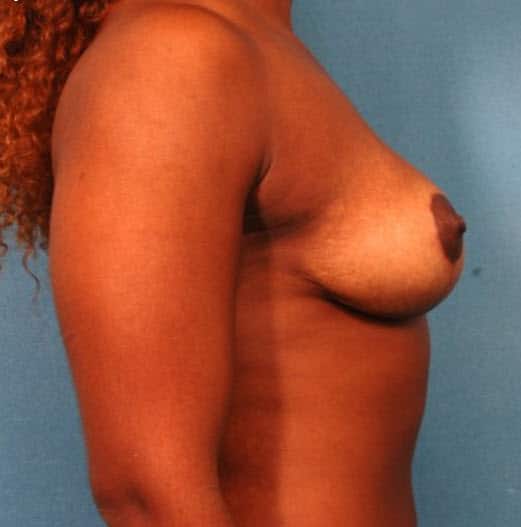
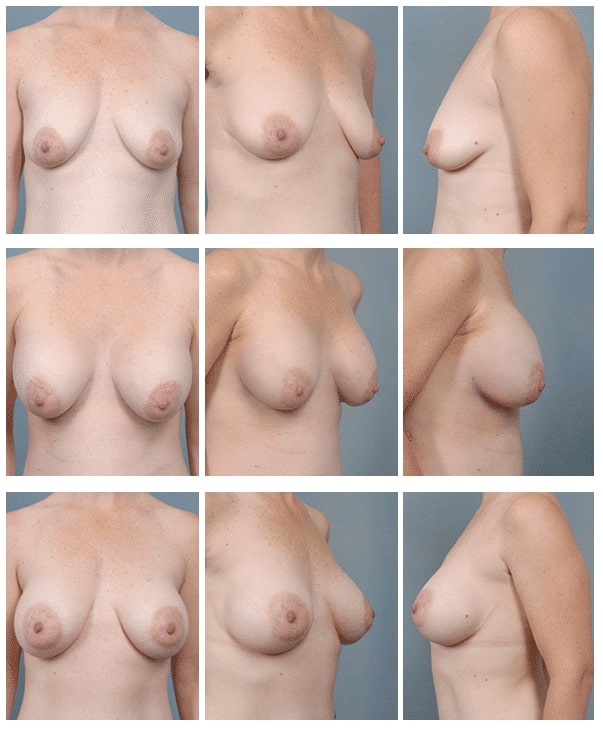
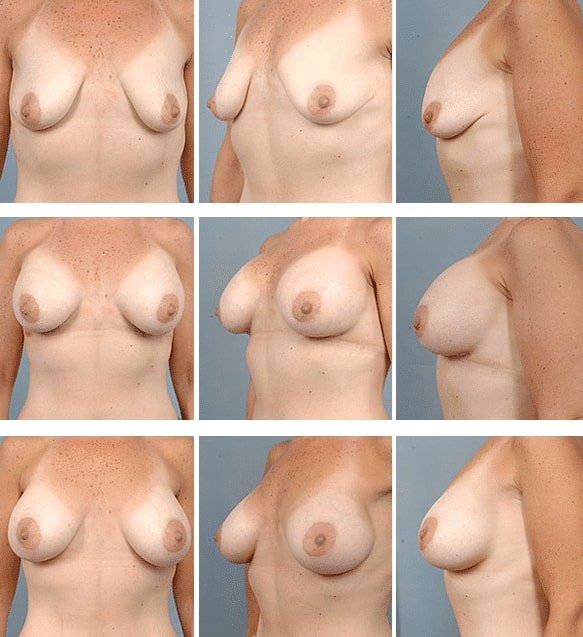
Below are several different cases illustrating different variations of anatomy, skin and breast tissue quality, and nipple position. As you view the cases, there is a worsening in the progression of breast ptosis (sagging). In the first three cases, there is mild glandular ptosis (drooping) but the nipple is still in an adequate position. When only the breast glandular tissue is sagging and the nipple is still in the correct position, we call this type of ptosis "pseudoptosis." I was able to correct the mild glandular ptosis using only a Dual Plane technique. This is achieved through the standard breast crease incision used to place the implant. No additional incisions are required. It involved repositioning the pectoralis major muscle. There is no need to reposition the nipple.
Then there is more severe ptosis of the breast gland in addition to ptosis of the nipple (nipple is too low), then a breast lift is required in addition to the augmentation. Click on the word "case" in each example to see an entire set of photos from all views for that patient with a description of that case.
The Scars
The technique required for a breast lift will be based upon an accurate assessment of the anatomy of the breasts and the degree of breast ptosis as discussed immediately above. The scars required to lift the breast vary based upon the technique required. At the very minimum, if the only issue is that the nipple is a little bit low, the nipple itself will need to be repositioned and that will require a scar around the areola (the round disc of skin surrounding the nipple itself). This is called a periarolar mastopexy (breast lift). Sometimes, when the nipple is a little lower, and there is excess skin from the lower portion of the breast that needs to be removed with the addition of support (and possibly removal) of some of excess breast tissue in the lower breast. If this is mild to moderate in extent, the incisions required are now around the areola along with a vertical scar from the bottom of the areola to the lower breast crease. This is called a circumvertical mastopexy, also known as a "lollipop lift." When the nipple is even lower, and the degree of excess skin is greater along with the amount of sagging of the glandular tissue in the lower breast, we need to add one more scar - in the lower breast crease. The length of this scar will vary depending upon the extent of the deformity. A breast lift that requires a scar around the areola, a scar from the bottom of the areola to the lower breast crease AND a scar in the lower breast crease is called a "Wise pattern mastopexy" or "Anchor pattern."
Making the Decision
Sometimes, the decision is so obvious that a breast lift is needed that every lay person will agree that a breast lift is in fact needed. Other times, the need for a breast lift is not so obvious. Breast drooping is not an "all or none" phenomenon, as you can see from the past section and again you will find below, breast drooping lies on a spectrum from mild to severe. As discussed, there is a classification system created to stratify the degree of drooping (ptosis), and this does help in making the decision. Understand, no one "needs" a breast lift (mastopexy). It is needed if you want your breasts to appear to lie within certain "aesthetic ideals"; that is, what most women would want there breasts to look like. For a woman with breasts pointing downward (Grade III Ptosis), certainly most women would want a breast lift. If you are placing implants into breasts that point downward, the result is going to lie far away from what most women would consider acceptable or desireable. Certainly, if you do not desire a breast lift but just want the volume of the implants, there is no "breast police" out there that will call you out for making such a decision.
In other cases, when there is more mild ptosis, the decision to proceed with a lift can be more flexible. Again, if a woman is desirous of a breast augmentation, but there is only very mild ptosis, she can rest assured that her breasts will look great supported in a bra or bathing suit top. It is only when she is undressed, that the overall shape of the breast and the position of the nipple may be a bit low. During such consultations, I have often heard a woman say "it is just me and my husband who will see me naked. Neither of us really care about the small amount of drooping of the breast, I would rather accept that and not have the additional scars required with a breast lift." In this case, I perform only the breast augmentation and not the lift.
When is a Breast Lift Needed with Implants?
Selecting the Correct Technique
Sometimes at consultation a woman will have already done a fair amount of research on her own, usually via the internet, which I wholeheartedly support. Maybe they also had other previous consultations. Sometimes the consultations were with skilled and knowledgable breast surgeons and in such cases, my opinion is usually concurs with what the patient has been previously told. Sometimes this is not the case, and the patient is recommended a procedure in which I am not in agreement with. This is a little harder situation, because I have to spend additional time educating the patient as to why my recommendation is better than the other surgeon's. While I do not mind spending this additional time with the patient; I actually thoroughly enjoy educating my patients, it is a cause for confusion to the patient. The the patient needs to make a decision as to which surgeon is more credible.
Occasionally, the patient will agree that they need a lift, and they will ask "do you do the <fill in your choice of a procedure> technique?" Usually, this is the technique with the least amount of scarring - the periareolar technique. The answer is that I do all the techniques, but one size does not fit all. Neither surgeon nor patient wants to subject the patient to additional scarring, but the fact of the matter is that you cannot get an adequate result when using a smaller scar procedure when the patient's anatomy dictates otherwise.
As a general guideline, and this is only an approximation, I use these guidelines as a starting point. They are subject to modification based upon a thorough analysis of the entire breast anatomy and tissue qualities, along with the desires of the patient.
If NOT performing a simultaneous breast augmentation with implants:
- No nipple ptosis, mild to moderate pseudoptosis (glandular ptosis) - No breast lift is required.
- Grade I nipple ptosis, mild pseudoptosis - Periareolar breast lift to reposition the nipple. No need to treat the mild glandular ptosis in the lower breast.
- Grade I nipple ptosis, moderate pseudoptosis - Circumvertical breast lift to reposition the nipple, the vertical scar is needed to manage the drooping gland in the lower breast.
- Grade II nipple ptosis, moderate pseudoptosis - Circumvertical breast lift to reposition the nipple, the vertical scar is needed to manage the drooping gland in the lower breast.
- Grade II nipple ptosis, severe pseudoptosis - Wise pattern breast lift to reposition the nipple, the vertical and lower breast crease scars are needed to manage the more extensive drooping gland in the lower breast.
- Grade III nipple ptosis, severe pseudoptosis - Wise pattern breast lift to reposition the nipple, the vertical and lower breast crease scars are needed to manage the more extensive drooping gland in the lower breast. The nipple usually needs to move a greater distance upward and the additional skin excision provides the room to do this without creating deformity of the areolar shape.


In the above case, there is second degree ptosis with a moderate amount of breast tissue below the level of the inframammary crease. A circumvertical ("lollipop") breast lift technique was chosen. There is no implant.


In the above case, there is second degree ptosis with a more severe amount of breast tissue below the level of the inframammary crease. A Wise pattern ("anchor") breast lift technique was chosen. There is no implant.
In the above case, there is third degree ptosis with an even greater amount of breast tissue below the level of the inframammary crease than in the first two cases. A Wise pattern ("anchor") breast lift technique was chosen. There is no implant.
Why did I not show a periareolar lift? The reality is that a periareolar lift is for the most minor amounts of breast drooping. Most women I have encountered who have such little drooping and do not want an implant, will not accept a visible scar around the areola just to correct a small amount of ptosis. This technique is very helpful when performing a simulataneous breast augmentation with implants and it is desired to optimize the placement of the areola on the now augmented breast. It is also useful in cases of asymmetry where only one side needs a periareolar lift or one side needs a circumvertical lift on one side and a periareolar lift on the other side to improve symmetry.
For Those Interested in a Breast Lift With Implants, Please Read the Information Below
Again, I want to reiterate here that it is a common misconception that breast implants lift the breast. They do not. The extra volume provided by breast implants does take up some of the slack from a loose breast skin envelope and will alter the amount of skin removal required to lift the breast. In some cases, it may change the technique required to lift the breast. Below is an approximate algorithm I use to decide which breast lift procedure is indicated when combining a breast lift with breast implants.
If performing a simultaneous breast augmentation with implants:
- No nipple ptosis, mild to moderate pseudoptosis (glandular ptosis) - Dual Plane II or III breast augmentation procedure.
- Grade I nipple ptosis, mild pseudoptosis - Periareolar breast lift with a Dual Plane II breast augmentation procedure.
- Grade I nipple ptosis, moderate pseudoptosis - Periareolar breast lift with a Dual Plane III breast augmentation procedure.
- Grade II nipple ptosis, moderate pseudoptosis - Circumvertical breast lift to reposition the nipple (the vertical scar is needed to manage the drooping gland in the lower breast) with a Dual Plane II breast augmentation procedure.
- Grade II nipple ptosis, severe pseudoptosis - Wise pattern breast lift to reposition the nipple (the vertical and lower breast crease scars are needed to manage the more extensive drooping gland in the lower breast) with a Dual Plane II breast augmentation procedure.
- Grade III nipple ptosis, severe pseudoptosis - Wise pattern breast lift to reposition the nipple (the vertical and lower breast crease scars are needed to manage the more extensive drooping gland in the lower breast) with a Dual Plane II breast augmentation procedure. The nipple usually needs to move a greater distance upward and the additional skin excision provides the room to do this without creating deformity of the areolar shape.
Why the Dual Plane Procedure?
Many surgeons when presented a woman with glandular ptosis will recommend a subglandular (above the muscle) augmentation as opposed to a submuscular (below the muscle) augmentation. This is to avoid a deformity of lower breast sagging when placing the implant below the muscle. While a subglandular approach will avoid this deformity, which amost looks like a "snoopy nose", such an apprach has other disadvantages when compared to the submuscular approach, particularly impacting the appearance of the upper breast and with time sometimes developing a strong outline of the implant under the breast, especially with larger implants. Some surgeons who are more desirous of a submuscular placement for the implant will then add a breast lift to correct the lower part of the breast, even though the nipple position is adequate. For this reason, the Dual Plane submuscular breast augmentation procedure was devised by John Tebbetts and published in 2001. It has impacted my breast augmentation practice hugely and for the better!
The Dual Plane procedure is used only when placing breast implants into the submuscular (below the muscle) position, which is usually my preference, as opposed to above the muscle. When placing implants below the muscle, it is not desireable to have complete coverage of the entire implant by muscle, or else the breast will look high and round like half a melon stuck to the chest. While the upper part of the implant is covered by the pectoralis major muscle with the breast parenchyma (glandular and fatty tissue and skin) overlying the muscle, the lower portion of the implant is only covered by breast tissue. This is not a bad thing. This is what makes the breast appear natural. The Dual Plane procedure is a repositioning of the lower edge of the pectoralis muscle upwards. This results in less of the upper breast implant being covered by muscle and more of the lower breast implant being covered by breast only. What this does is allow the lower breast to expand better under the influence of the implant in situations where there is mild to moderate pseudoptosis (glandular drooping). The end result is a more full lower pole (portion) of the breast with a more pleasing appearance.
In my practice, the Dual Plane submuscular augmentation has clearly reduced the number of breast lifts I would have otherwise have done with my augmentations. Similarly, it has, in my opinion, eliminated the need for placing implants above the muscle (subglandular) in cases where there is glandular ptosis or drooping. The advantage to this technique is that even though the implant has less muscle coverage, the implant is remains covered at the upper third. This results in a more pleasing appearance to the breast where the upper breast border takes off from the chest wall. This gentler transition affords a more natural appearance to the breast. So in summary, Dual Plane submuscular augmentation leverages the best qualities of a submuscular breast augmentation with those of a subglandualr breast augmentation. It is still considered a "below the muscle approach", and in my opinion, affords the very best results.
IMPORTANT: when a breast lift is required, I use the Dual Plane procedure to reduce some of the "loading" at the lower part of the breast - to mitigate the lower breast tissue drooping, and also perform a breast lift to reposition the nipple and optimize the overall distribution of breast tissue in the breast.
With all the Above Information Noted, When is a Breast Lift Actually Needed at the Time of Breast Augmentation?
I frequently see women who have been told by other plastic surgeons that they require a lift in addition to the breast augmentation surgery. Many of these women DO NOT require a breast lift. Using some of the latest advances and refinements in breast pocket dissection, coupled with proper implant size and shape selection, the implant can be fitted into the breast pocket so as to restore lost fill volume to the breast, thus advancing the nipple forward and rotating it upward. In these cases a lift is not necessary. Sometimes the reverse is the case. I have had patients tell me that other surgeons have told them that they do not require a lift, but one is in fact necessary to achieve ideal breast aesthetic ideals.
This cannot be achieved in every case, however, after a thorough analysis of the breast and careful measurements, the need for a mastopexy (breast lift) usually can be determined during the initial consultation. In other cases, such as when the nipples are at the lowest point on the breast when standing or if the nipples point straight downward, a lift is often unavoidable. In borderline cases, I have found it very helpful to perform the augmentation first, and allow the implants to settle into place. Six months later, if a lift is required, this can be performed. In my experience with these types of cases, a breast lift is almost never required or desired by the patient six months later.
I think everyone would agree that a small, tight, perky breast with the nipple positioned centrally on the breast, well above the lower breast crease will not need a lift when an augmentation is performed. On the other hand, in a case where the breasts have very saggy skin with poor elasticity, breast tissue that is not firm but in excess and the nipples point straight downwards, everyone will easily agree that a lift is definitely indicated in this case. The issue remains, what to do for everyone in the middle? This becomes a judgment call, based upon experience. That experience comes from performing thousands of surgeries, and seeing what works and what does not work.
The last thing that I want to state is that a combined breast augmentation and lift is one of the more challenging surgical procedures in plastic surgery. It is not at all technically difficult for an experienced surgeon. The challenge comes from dealing with compromised breast tissue that will stretch in sometimes unpredictable ways, placing an implant into those tissues and then removing skin and rearranging tissue so that after all these many variables come into play, one ends up with a pleasing aesthetic result. This only happens by a great deal of experience and technical skill!
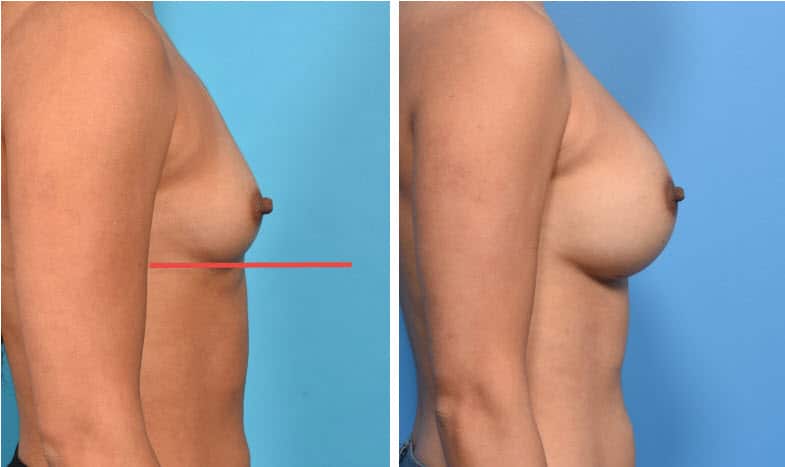
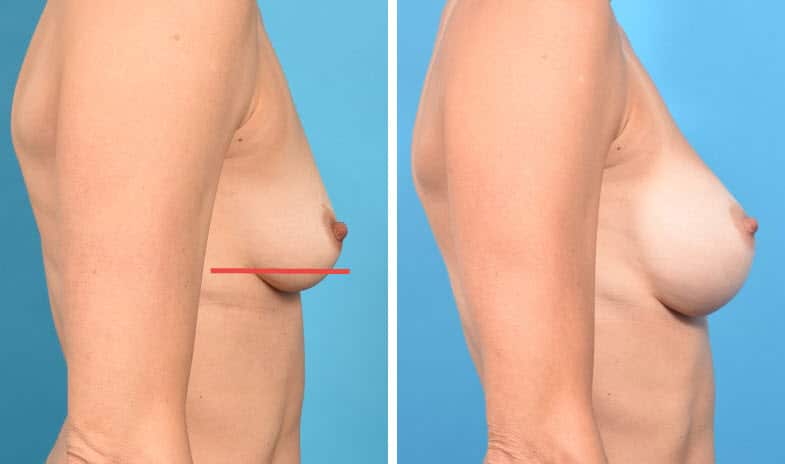
In the above case, the breast is small, tight, young, no history of pregnancy. There is minimal breast tissue, no excess of skin, breast tissue and skin of excellent quality, nipple in perfect position above the crease on the most projecting forward portion of the breast. No breast tissue lies below the lower breast crease (red line). Dual Plane I pocket for the implant. No lift is needed.
In the above case, the breast is a little larger, slightly lax, young, no history of pregnancy. There is a moderate amount of breast tissue, no excess of skin, breast tissue and skin of very good quality, nipple in perfect position above the crease on the most projecting forward portion of the breast. A small amount of breast tissue is lying below the lower breast crease, but the nipple is still well above it. Dual Plane II pocket for the implant. No lift is needed.
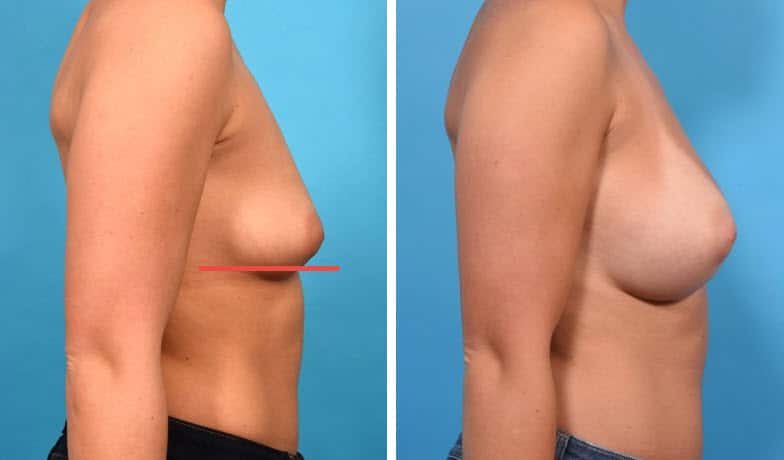
In the above case, the breast is still of small size, there is no excess of breast skin. The skin has less elasticity, and the breast tissue has poorer quality than the above examples. More of the breast is now lying below the lower breast crease. Dual Plane III pocket for the implant. Still, no lift is needed.
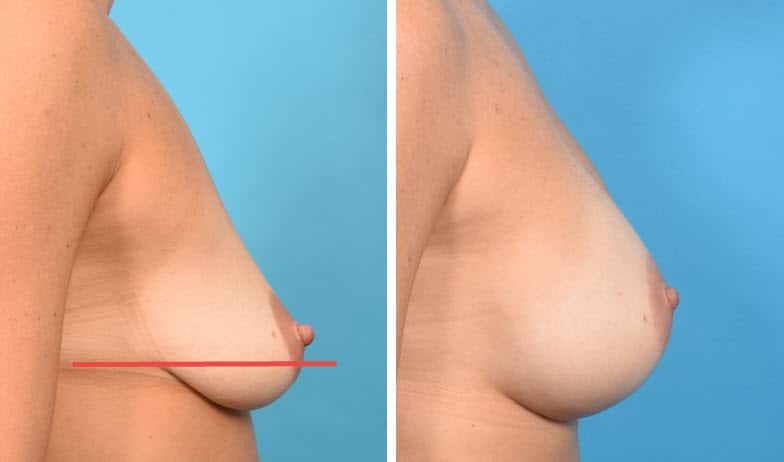
In the above case, the nipple itself is still slightly above the crease, but there is slightly more breast tissue and excess skin than the previous case studies, and the tissue quality of each is more compromised. More tissue lies below the crease, and the nipple lies very close to the crease, even though still on the most projecting portion of the breast. In this case, a lift was essential. I created a Dual Plane I pocket for the breast augmentation and a circumvertical ("lollipop") mastopexy (breast lift) where the scar is around the nipple and also from the lower portion of the nipple to the lower breast crease.
In the above case, the nipple is above the crease, but not quite as high as desired. The areolar diameter is also a little larger than ideal. There is minimal breast tissue below the lower breast crease. A Dual Plane I submuscular pocket was used for the breast augmentation and a periareolar mastopexy (breast lift) where the breast lift scar is limited to around the areola only.
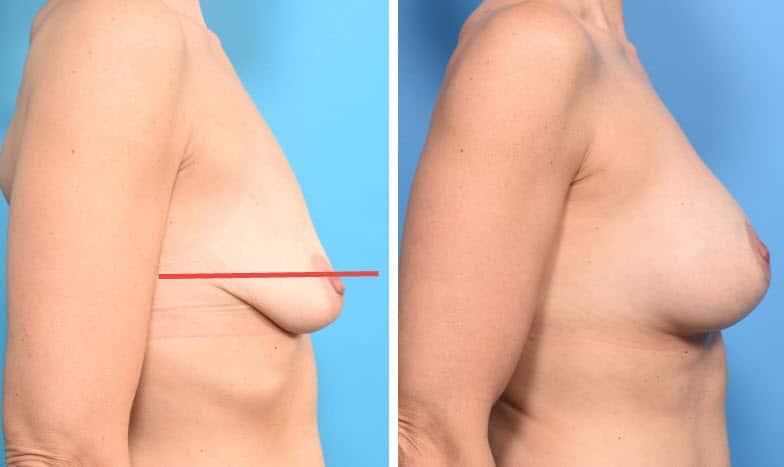
In the above case, the situation is similar to the case above, except that there is more excess skin with less elasticity, most of the breast is breast is now below the lower breast crease, the nipple is also slightly below the crease (grade I ptosis), the breast tissue is more compromised than any of the above cases. A Dual Plane II pocket was created for the augmentation, along with a circumvertical ("lollipop") mastopexy (breast lift).


In this case, there is more ptosis (Grade II) and pseudoptosis. Tissue quality is fair. As in the preceding case, there is approximately half the breast below the crease, but the degree of nipple ptosis is greater. A Dual Plane II pocket was created for the augmentation, along with a Wise pattern ("anchor") mastopexy (breast lift).
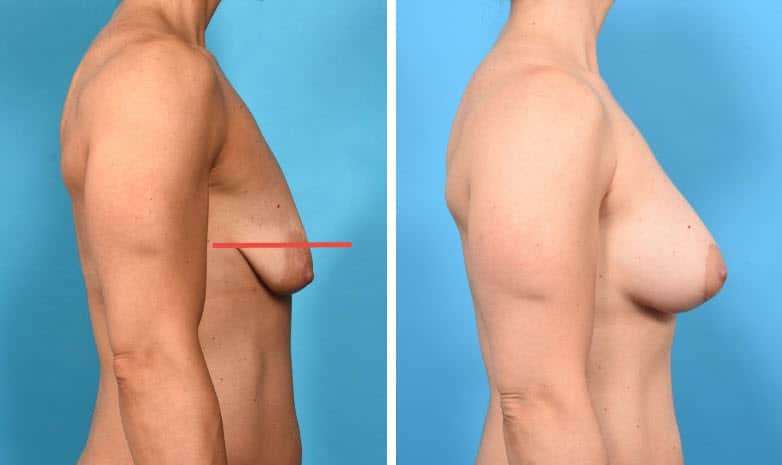
This case represents an even more exaggerated sagging of the breasts with all of the breast tissue lying below the breast crease, breast tissue is of very poor quality, nipple is well below the crease and now pointing downward. There is marked excess breast skin with extremely poor elasticity. In this case, I created a Dual Plane II pocket for the breast augmentation along with a circumvertical ("lollipop") mastopexy (breast lift).
Is a Breast Lift Performed at the Same Time as the Augmentation?
Breast lift and augmentation can be performed in one or two stages. In the vast majority of cases, I prefer to perform the two procedures at the same time. As I can get predictably excellent results, why subject the patient to two separate surgical procedures?
There is a special situation where I make an exception to this rule. When there is a very significant difference in breast size, breast shape and nipple position (drooping/ptosis), I find it better to do this in two stages for more accurate and consistent results. The key is the word "consistent." Then the breasts are of a significant difference in both size and shape with one breast more ptotic (drooping) than the other, it is very hard to address the differences in breast volume, skin envelope and breast shape accurately in one operation. There are just too many "variables." A variable is an issue the surgeon does not have complete control over because healing, scarring and tissue stretching come into play, and these things both the patient and surgeon cannot control. If a surgeon tries to attempt to correct all differences in size, shape and nipple position in one operation, they might get away with it once, but if they did a large number of these, then many of them would most likely not look so good, or not look as hoped. When I do a surgery, I want a very high likelihood that the result will turn out to look good and as I had hoped it would. It's all about the surgeon maximizing his control of the procedure.
The way I address this is to correct the issues of size disparity, shape, and nipple position with one procedure. What I am not going to attempt is to add extra volume with an implant at the same time. The shape, size and weight of the implant will make the "variables" here too difficult to predict/control, leading to unpredictable results which will vary from excellent (unlikely) to suboptimal (more likely) to poor. While you can theoretically go back later and revise an unsatisfactory result, that subjects the patient to another procedure which is probably going to yield a result less satisfactory than if everything came out optimal the first time. Now you understand my logic and decision making. Surgery is not just about technique; just as important is decision making and selection of proper technique.
In this particular situation, I like to perform a standard breast reduction on the larger breast. Keep in mind that every single breast reduction includes a lift. So when we say "breast reduction", we mean "breast reduction and lift", but we do not say that because it is implied that the reduction includes a lift. This is almost always performed using a circumvertical scar, so the scar is around the areola and a small vertical scar from the bottom of the areola to the lower breast crease. Both scars heal very well in the vast majority of cases, and what few do not, we can optimize with lasers. Now I have reduced the size of the breast so that it is approximately that of the smaller breast, I have also elevated the nipple/areola to match the smaller breast as well. There usually is some small residual difference in volume, but this is not more typical of what I usually see in my regular breast implant patients.
After four to six months when the reduced breast is now healing well, I can then perform a breast augmentation in the usual fashion, often putting a slightly smaller implant in the reduced breast because usually the reduced breast ends up being slightly larger than the other breast. If the reduced breast is smaller, than that breast will receive a larger implant. Very rarely are the two breasts the same exact size (within 30 cc - 1 ounce) after the breast reduction. They do not have to be the same size anyway, as using two slightly different implant sizes will yield two very similar looking breasts.
This is illustrated by the case shown below. More examples of two stage reduction/augmentation procedures can be found here.

Performing the augmentation first and the lift later is extremely uncommon. The only situation where that would occur is if either I was not 100% certain the patient needs a lift. In this case, I would perform the augmentation, wait six or so months and then reassess to see if a lift is needed. This is in cases where the amount of sagging is mild and the patient is on the borderline for needing a lift. So far, I have yet to have to go back on any of these patients and do a lift at a later date - the Dual Plane procedure has always taken care of the problem. The other situation to perform the augmentation first and the lift later is when the patient is not sure if they want the lift because of the extra scar around the nipple (as in all lifts) and from the nipple to the lower breast crease (as in most lifts). In this case, again, the augmentation is performed first, and then the patient reassessed in six months to see if a lift is needed (or desired by the patient). Some patients are fine with a little sagging, they just want to avoid the extra scars. The majority of my patients are not concerned about the scars from a breast lift because they heal so well and the improvement in breast contour is for these patients a much greater benefit.
Two Cases Where I Did Not Perform a Breast Lift at the Time of Augmentation - Maybe I Should Have???
Below are two case studies of women who desired breast augmentation but did not want a breast lift. Both women had substantial deflation of their breasts following lactation with Grade II ptosis - their nipples were approximately at the level of the lower breast crease (the second case is a little more severe than the first case). In both cases, I did not perform a breast lift. What I did do to address the glandular ptosis (pseudoptosis) was to perform a Dual Plane III pocket dissection, repositioning the lower portion of the pectoralis muscle a little higher over the implant. The implant is still under the muscle on its upper portion, but the lower portion does not have as much muscle coverage. The upper muscle coverage preserves the natural transition from upper chest wall to the breast on the upper breast, but allows the implant to better take up the slack of the excess skin envelope on the lower breast. I think I achieved a very nice result in these short term follow up photos. I would be curious to know how the breasts look over fifteen years later since surgery. The issue of concern is not only the skin, but also the poor quality breast tissue contained within.
What I have learned over the past three decades of performing this type of surgery is that the implant merely pushes the entire breast forward, it does not lift the breast. When there is little breast tissue to start with, there is not much tissue to sag later on. The concern is when there is more breast tissue, tissue that is already compromised and not as firm as it once was. This tissue may look fine without a lift as it does in these two below cases. However, with the passage of time, this tissue will start to sag, often taking the nipple along for the ride! The more breast tissue you are trying to manage using a Dual Plane approach and no lift, the more at risk that tissue is to "slide off the front of the implant" and sag later on. The take away message her is that when there is more breast tissue of poor quality to deal with, the threshold to decide to incorporate a breast lift into the plan needs to be lower. This is a judgment call and is based upon extensive experience with breast augmentation.
Patient Information: 32 year old female show pre-operatively, 2 days after submuscular placement of 339 cc round silicone gel filled implants placed via a Dual Plane III technique, and 5 months later. Note how the volume of the implant redistributes with time to the lower portion of the breast, rotating the nipple upward. Also, the excessive upper breast fullness corrects as well. Without a dual plane approach, this degree of correction with time could not be achieved. NO LIFT WAS REQUIRED!
Patient Information: 40 year old female show pre-operatively, 2 days after submuscular placement of 400 cc round silicone gel filled implants placed via a Dual Plane III technique, and 4 months later. Preoperatively, these breasts are severely "deflated", or demonstrate marked volume loss with relative skin excess. After surgery, note how the volume of the implant redistributes with time to the lower portion and especially the anterior portion of the breast, moving the nipple forward and rotating it upward. Note how the excessive upper breast fullness resolves. Without a dual plane approach, there would be a severe "Snoopy dog" deformity of the breasts, where the breast tissue would hang off the front of the implant. Again, NO LIFT WAS REQUIRED!
My concern for both of these cases is that the results are shown only a short while after surgery. The big question is how would these woman look 1, 2 and 5 years after surgery??? Unfortunately, I do not have longer term follow up on these women.
SECTIONS - Breast Lift/Mastopexy with Implants
Chapters - Breast Augmentation Guide
- Intro to Breast Augmentation
- Motiva Breast Implants
- Five key decisions you need to make
- One-Day Recovery Breast Augmentation
- Anesthesia – General, Sedation or Local?
- Breast Lift (Mastopexy) with/without Implants or Fat
- What else should I know about breast augmentation?
- Important Things to Consider When You Decide to Move Forward With Breast Augmentation
- Revision of breast augmentation
- ALCL and Breast Implant Illness


