Introduction
Next to implant size, this is probably the biggest concern my patients have. Most of my patients do not need a lift. They realize this, and so it never comes up for discussion. Some of my patients need a lift, and fortunately, they know this. The problem is when a patient comes in and needs a lift, but they were not prepared to hear me recommend this. Sometimes, they take it well and it’s a non-issue. Sometimes, they are fearful to move forward because of the extra scars or the cost becomes prohibitive. For those patients, I feel badly because it is like being hit with a ton of bricks. They just were not prepared for this.
I could write a book chapter on this subject. I do believe that breast lifts are sometimes over-utilized. In other words, I believe that some women are getting them when they do not need them. I was once attending a presentation on breast augmentation. A series of questions were asked of the audience, and each of us was able to respond using a little hand-held remote to cast our vote. The results were then instantly tallied and displayed on the screen for all to see in real time. Pretty amazing technology. One of the questions asked was “what percentage of your first time augmentations do you do a breast lift at the same time?” The answers varied from 4% to 80%. I would assume, that on average, each surgeon probably sees a similar mix of patients, so why do some surgeons do very few breast lifts with their augmentations and others do a lot of them? I would assume that some surgeons are under-utilizing breast lifts and some are over-utilizing them.
The Problem: Breast Drooping
True Ptosis versus False Ptosis (Pseudoptosis)
In my breast augmentation practice, a large portion of my patients are mothers who wish to restore lost volume to their breasts, or attain a volume that they wished they had previously. Many of these women have ptosis, or drooping, of their breasts. There are two types of ptosis: true ptosis and false ptosis, also known as pseudoptosis. True ptosis relates to the position of the nipple with respect to the lower breast crease, also known as the inframammary fold. False ptosis describes the position of the glandular tissue with respect to the inframammary fold. The degree of ptosis and pseudoptosis can vary independently with respect to one another as they are two separate entities. Unfortunately, they happen to have similar names which causes the confusion. Except for those women with very little breast tissue to start with, most all of these women have a combination of both types of ptosis.
In my practice, the Dual Plane submuscular augmentation has clearly reduced the number of breast lifts I would have otherwise have done with my augmentations. Similarly, it has, in my opinion, eliminated the need for placing implants above the muscle (subglandular).
So with these things said, when do I do a lift?
I frequently see women who have been told by other plastic surgeons that they require a lift in addition to the breast augmentation surgery. Many of these women DO NOT require a breast lift. Using some of the latest advances and refinements in breast pocket dissection, coupled with proper implant size and shape selection, the implant can be fitted into the breast pocket so as to restore lost fill volume to the breast, thus advancing the nipple forward and rotating it upward. In these cases a lift is not necessary.
This cannot be achieved in every case, however, after a thorough analysis of the breast and careful measurements, the need for a mastopexy (breast lift) usually can be determined during the initial consultation. In other cases, such as when the nipples are at the lowest point on the breast when standing or if the nipples point straight downward, a lift is often unavoidable. In borderline cases, I have found it very helpful to perform the augmentation first, and allow the implants to settle into place. Six months later, if a lift is required, this can be performed. In my experience with these types of cases, a breast lift is almost never required or desired by the patient six months later.
Watch the video below for some insights on this topic:
I think everyone would agree that a small, tight, perky breast with the nipple positioned centrally on the breast, well above the lower breast crease will not need a lift when an augmentation is performed. On the other hand, in a case where the breasts have very saggy skin with poor elasticity, breast tissue that is not firm but in excess and the nipples point straight downwards, everyone will easily agree that a lift is definitely indicated in this case. The issue remains, what to do for everyone in the middle? This becomes a judgment call, based upon experience. That experience comes from performing thousands of surgeries, and seeing what works and what does not work.
Five factors that determine the need for a lift at the time of augmentation
- The amount of excess breast skin – the more excess skin, the greater the likelihood to need a lift
- The elasticity of the breast skin – the poorer the elasticity, the greater the likelihood to need a lift
- The amount of the breast tissue – the more breast tissue, the greater the likelihood to need a lift
- The firmness of the breast tissue – the softer the breast tissue, the greater the likelihood to need a lift
- The position of the nipple relative to the lower breast crease – the lower the nipple, the greater the likelihood to need a lift
If you envision a breast with an implant behind it, the breast tissue is pushed forward of that implant. Gravity is going to act on that breast tissue. The more factors that are unfavorable, the more the breast will sag and will thus need a lift to restore proper aesthetics to that breast.
With regard to the skin envelope, think of it as a ziploc bag. If the bag has a capacity for a gallon, but you fill it with only one quart of water, all the water will fall to the bottom of the bag, leaving the majority of it unfilled and sagging. Same thing with a breast. If the skin brassiere (the skin envelope) has a DD-cup capacity because that is the size you were while breast feeding, but now you only have a B-cup of breast tissue to fill it, the breast will appear empty and sagging. It is a common misconception to think that adding an implant to make up the difference will remedy the matter. Furthermore, an implant DOES NOT lift the breast. The problem is that the skin is overstretched and has poor elasticity. If you add a very large implant to fill out the breast, the nipple will appear too low, and the weight of this very large implant will now cause additional thinning out of the skin and stretching, and in a few months the breasts will look even worse! The answer here is to remove some of the breast skin (as is done with a breast lift) and make the skin envelope smaller with the nipple now in the proper position, use a smaller implant and get a much longer lasting result, maybe a C or D-cup with the breast properly filled out and the nipple positioned properly.
With regard to the breast tissue itself, the more breast tissue there is to start, the more it will be pushed forward of the implant. Gravity will act on this tissue, causing it to sag. The firmer the tissue, the more it will resist deformation of shape under the influence of gravity. The more tissue to start with, the firmer it must be to stay upwards.
The nipple position is also a very important factor. Ptosis, or drooping, is always assessed by looking at the nipple position in relation to the lower breast crease, also known as the inframammary fold. I do not care what the measurement is from the collar bone or the upper breast bone at the base of the neck to the nipple when assessing ptosis. Only the crease. Of course, I record these measurements, but more for symmetry purposes than any other reason. Very simply stated, the breast is like a hemisphere, and we want the nipple to be placed on the part of the breast that projects forward the most. This should be approximately the center of the breast. You cannot reference what the center is unless you can also see what the bottom of the breast is (where the lower breast crease is).
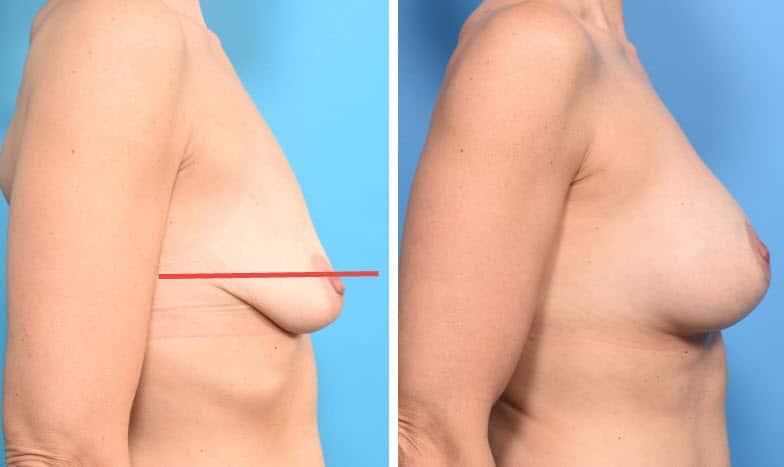
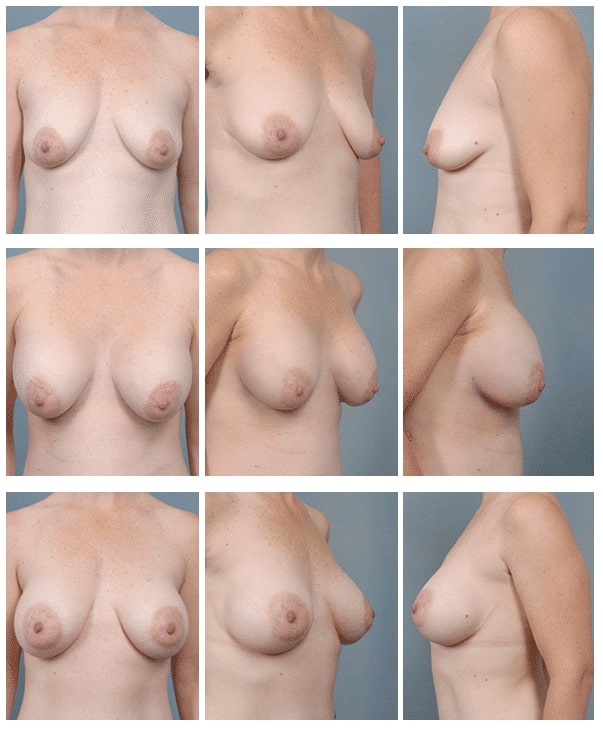
Below are several different cases illustrating different variations of anatomy, skin and breast tissue quality, and nipple position. As you view the cases, there is a worsening in the progression of breast ptosis (sagging). In the first three cases, there is mild glandular ptosis (drooping) but the nipple is still in an adequate position. When only the breast glandular tissue is sagging and the nipple is still in the correct position, we call this type of ptosis “pseudoptosis.” I was able to correct the mild glandular ptosis using only a Dual Plane technique. This is achieved through the standard breast crease incision used to place the implant. No additional incisions are required. It involved repositioning the pectoralis major muscle. There is no need to reposition the nipple.
Then there is more severe ptosis of the breast gland in addition to ptosis of the nipple (nipple is too low), then a breast lift is required in addition to the augmentation. Click on the word “case” in each example to see an entire set of photos from all views for that patient with a description of that case.
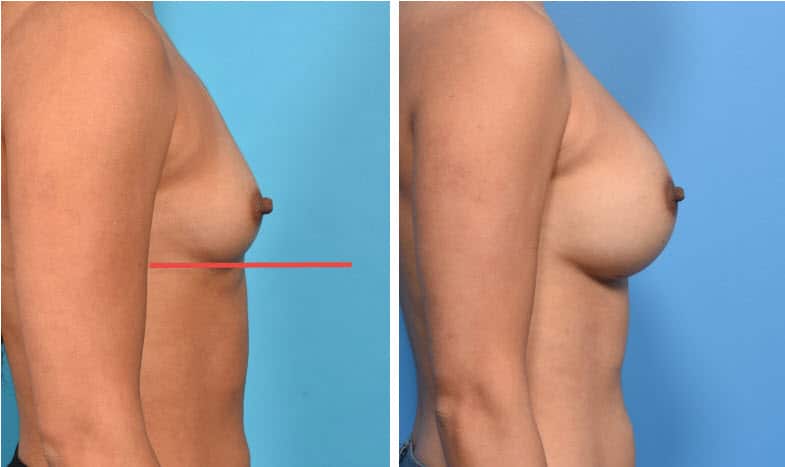
In the above case, the breast is small, tight, young, no history of pregnancy. There is minimal breast tissue, no excess of skin, breast tissue and skin of excellent quality, nipple in perfect position above the crease on the most projecting forward portion of the breast. No breast tissue lies below the lower breast crease (red line). Dual Plane I pocket for the implant. No lift is needed.
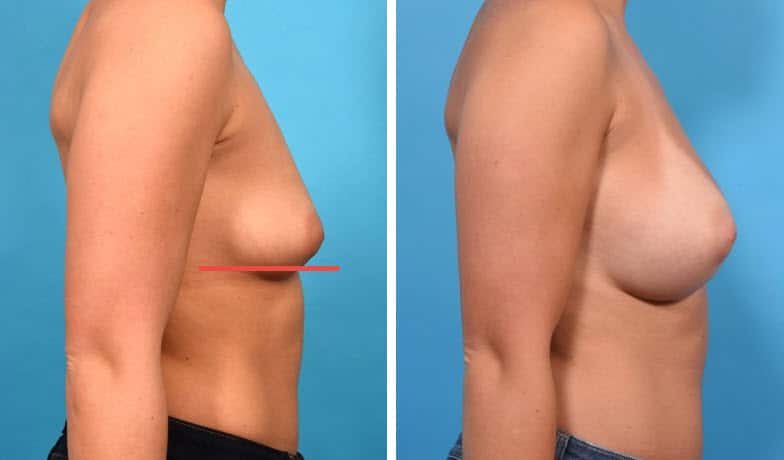
In the above case, the breast is a little larger, slightly lax, young, no history of pregnancy. There is a moderate amount of breast tissue, no excess of skin, breast tissue and skin of very good quality, nipple in perfect position above the crease on the most projecting forward portion of the breast. A small amount of breast tissue is lying below the lower breast crease, but the nipple is still well above it. Dual Plane II pocket for the implant. No lift is needed.
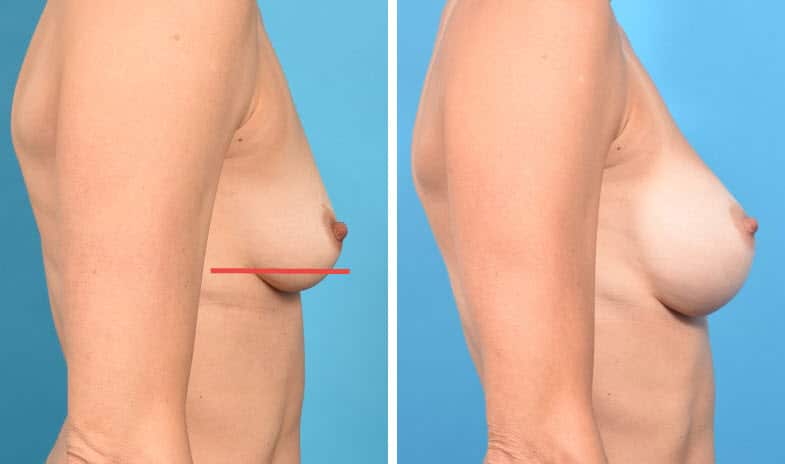
In the above case, the breast is still of small size, there is no excess of breast skin. The skin has less elasticity, and the breast tissue has poorer quality than the above examples. More of the breast is now lying below the lower breast crease. Dual Plane III pocket for the implant. Still, no lift is needed.
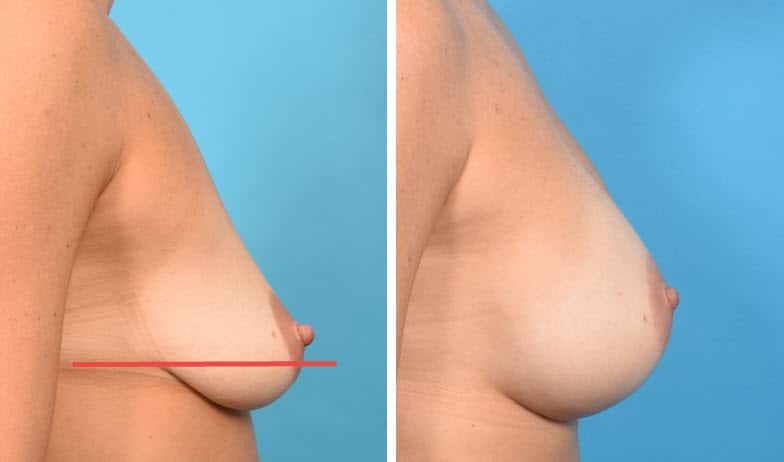
In the above case, the nipple itself is still slightly above the crease, but there is slightly more breast tissue and excess skin than the previous case studies, and the tissue quality of each is more compromised. More tissue lies below the crease, and the nipple lies very close to the crease, even though still on the most projecting portion of the breast. In this case, a lift was essential. I created a Dual Plane I pocket for the breast augmentation and a circumvertical (“lollipop”) mastopexy (breast lift) where the scar is around the nipple and also from the lower portion of the nipple to the lower breast crease.
In the above case, the situation is similar to the case above, except that there is more excess skin with less elasticity, most of the breast is breast is now below the lower breast crease, the nipple is also below the crease, the breast tissue is more compromised than any of the above cases. A Dual Plane I pocket was created for the augmentation, along with a circumvertical (“lollipop”) mastopexy (breast lift).
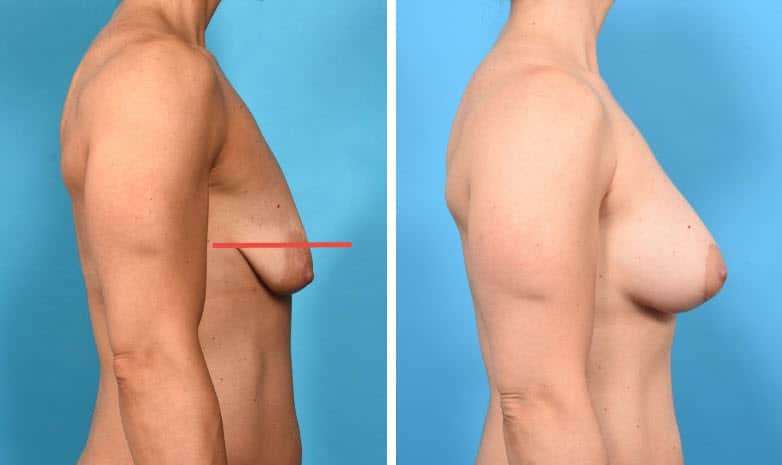
This case represents an even more exaggerated sagging of the breasts with all of the breast tissue lying below the breast crease, breast tissue is of very poor quality, nipple is well below the crease and now pointing downward. There is marked excess breast skin with extremely poor elasticity. In this case, I created a Dual Plane I pocket for the breast augmentation along with a circumvertical (“lollipop”) mastopexy (breast lift).
Two Cases Where I Did Not Perform a Breast Lift at the Time of Augmentation
Below are two case studies of women who desired breast augmentation but did not want a breast lift. Both women had substantial deflation of their breasts following lactation with Grade II ptosis – their nipples were approximately at the level of the lower breast crease (the second case is a little more severe than the first case). In both cases, I did not perform a breast lift. What I did do to address the glandular ptosis (pseudoptosis) was to perform a Dual Plane III pocket dissection, repositioning the lower portion of the pectoralis muscle a little higher over the implant. The implant is still under the muscle on its upper portion, but the lower portion does not have as much muscle coverage. The upper muscle coverage preserves the natural transition from upper chest wall to the breast on the upper breast, but allows the implant to better take up the slack of the excess skin envelope on the lower breast.
Patient Information: 32 year old female show pre-operatively, 2 days after submuscular placement of 339 cc round silicone gel filled implants placed via a Dual Plane III technique, and 5 months later. Note how the volume of the implant redistributes with time to the lower portion of the breast, rotating the nipple upward. Also, the excessive upper breast fullness corrects as well. Without a dual plane approach, this degree of correction with time could not be achieved. NO LIFT WAS REQUIRED!
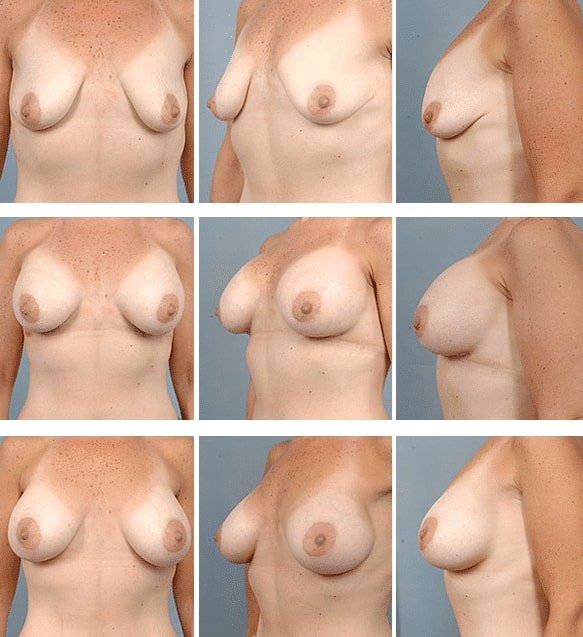
Patient Information: 40 year old female show pre-operatively, 2 days after submuscular placement of 400 cc round silicone gel filled implants placed via a Dual Plane III technique, and 4 months later. Preoperatively, these breasts are severely “deflated”, or demonstrate marked volume loss with relative skin excess. After surgery, note how the volume of the implant redistributes with time to the lower portion and especially the anterior portion of the breast, moving the nipple forward and rotating it upward. Note how the excessive upper breast fullness resolves. Without a dual plane approach, there would be a severe “Snoopy dog” deformity of the breasts, where the breast tissue would hang off the front of the implant. Again, NO LIFT WAS REQUIRED!
Is a breast lift performed at the same time as the augmentation?
Breast lift and augmentation can be performed in one or two stages. In the vast majority of cases, I prefer to perform the two procedures at the same time. As I can get predictably excellent results, why subject the patient to two separate surgical procedures?
When performing in two separate procedures, I prefer to perform the lift first. Otherwise, if performing the augmentation first, as the skin envelope is going to be larger than it would be had the lift been performed first, I might end up using a larger implant than I would otherwise use had I performed the lift first. This is more commonly done when I need to reduce one breast but not the other breast as well, such as in severe asymmetry procedures (case shown below).

Performing the augmentation first and the lift later is extremely uncommon. The only situation where that would occur is if either I was not 100% certain the patient needs a lift. In this case, I would perform the augmentation, wait six or so months and then reassess to see if a lift is needed. This is in cases where the amount of sagging is mild and the patient is on the borderline for needing a lift. So far, I have yet to have to go back on any of these patients and do a lift – the Dual Plane procedure has always taken care of the problem. The other situation is where the patient is not sure if they want the lift because of the extra scar around the nipple (as in all lifts) and from the nipple to the lower breast crease (as in most lifts). In this case, again, the augmentation is performed first, and then the patient reassessed in six months to see if a lift is needed (or desired by the patient). Some patients are fine with a little sagging, they just want to avoid the extra scars. The majority of my patients are not concerned about the scars from a breast lift because they heal so well and the improvement in breast contour is for these patients a much greater benefit.
Use of a Surgical Scaffold to Support the Lift
Breast tissue, like all living tissue, will stretch under the influence of gravity. In some of my patients, particularly the ones with the most compromised skin and breast tissue, I offer the option of using a surgical scaffold which is placed inside the breast to act as an “internal bra.” While this does add some time and cost to the surgical procedure, in these patients it is certainly worth this extra step to provide greater support to mitigate the effect of gravity and help ensure better, more long-lasting results to the lift. The particular product that I like to use for this is called GalaForm. This material is completely absorbable in about one to two years and is replaced with a new layer of scar tissue which continues to provide support for the breast. The safety and efficacy of this product is long established and I have a lot of experience using it.

The mesh is placed on the lower breast between the skin and the underlying breast tissue. The tabs allow the material to be easily sutured into place. The rim along its perimeter gives added support, much like the “underwire” in a bra. This video discusses the use of surgical scaffolds with breast lifts:
I do not recommend this for everyone, but when I do, it is because I am concerned about the longevity of the result of the breast lift. It is a wonderful option to offer to eligible women.
Is breast augmentation recovery longer when it includes a lift?
Patients are concerned as to whether or not adding a simulataneous breast lift (mastopexy) increases the downtime and duration of recovery. In my patients, I am not seeing much difference between breast augmentation alone and augmentation with mastopexy (lift) in terms of recovery time. Even though a breast lift performed at the same time as a breast augmentation requires longer incisions in total, the incisions only go down to the superficial tissues of the breast which heal quickly and with little discomfort. However, it is important to your recovery that you ambulate frequently during that time. I use a specialized “Recipe for Recovery” to hasten your recovery. After the procedure, it is often possible to return to work within one to three days.
Strenuous physical activity should be avoided for at least the first three weeks following surgery.
How your breasts will look and feel after a breast lift with implants?
Breast implants will add to the overall results of the breast lift procedure by lifting the breast and increasing your bust size in a single step*. Some discoloration and swelling may occur initially after the procedure, but this will disappear quickly.
After recovery, many women equate the feel of their breasts implants to that of a teenage girl with young, healthy, firm breasts. And when you undergo the breast augmentation combined with a breast lift, your breasts will typically remain full and perky for longer. It is important to understand that no surgery will change the quality of your breast tissue, so you will be feeling the breast tissue on top of the implant. The more natural tissue that you have, and the firmer that tissue is, the less you will be able to feel the implant itself. As today’s silicone gel implants are designed to mimic the feel of natural breast tissue, it becomes difficult at times to even feel the implant at all in some cases.
Risks And Complications Associated With A Breast Lift With Implants
All the risks applicable to a breast augmentation exist as well when augmentation is combined with implants. The main additional risks are that when the procedures are combined together, it may be difficult, if not impossible, to accurately predict where on the breast (at what height) the nipple will be positioned at after the breasts heal and the new shape stabilizes. This is due to the fact that tissue stretches after surgery and neither surgeon nor patient can either predict or control the amount of stretch that will occur. The reality is that the vast majority of such surgeries have excellent results with very happy patients (and surgeon!), but the patient still needs to understand this risk*. Another consideration is that there often will be some loss of correction of sagging, again due to tissue stretching (under the influence of gravity on the breast and implant) after surgery. Sometimes, I find that placing a piece of absorbable surgical mesh (Galaflex) on the lower part of the breast helps to reduce this problem.
Scarring After A Breast Lift With Implants
Scars are a part of the breast augmentation and mastopexy process. Fortunately, breast augmentation and mastopexy scars, regardless of where they are located, tend to heal extremely well. Scars following breast augmentation are usually small and inconspicuous, and Dr. Epstein will make sure the scar is as unnoticeable as possible. A mastopexy does add additional scars such as around the areola, and usually a vertical scar from the bottom of the areola down towards the lower breast crease. In some occasions, an incision is made in this crease, as well.
Breast Feeding After A Breast Lift With Implants
You will most likely be able to breastfeed after the breast lift with implants procedure, but it may depend on the kind of surgery you had and the type of incisions required.
Prev Section: What is a Breast Lift?
Next Section: How is a Breast Lift Performed?
SECTIONS - Breast Lift/Mastopexy with Implants
- What is a Breast Lift?
- Will I Need a Breast Lift (Mastopexy)?
- How is a Breast Lift Performed?
- The Use of Soft Tissue Support in Breast Lifts
- Recovery and Beyond After Breast Lift with Implants
Prev Chapter: Anesthesia - General, Sedation or Local? »
Next Chapter: What else should I know about breast augmentation? »
Chapters - Breast Augmentation Guide
- Intro to Breast Augmentation
- Motiva Breast Implants
- Five key decisions you need to make
- One-Day Recovery Breast Augmentation
- Anesthesia – General, Sedation or Local?
- Breast Lift (Mastopexy) with/without Implants or Fat
- What else should I know about breast augmentation?
- Important Things to Consider When You Decide to Move Forward With Breast Augmentation
- Revision of breast augmentation
- ALCL and Breast Implant Illness


